Have you ever wondered what goes on behind the scenes before a new medication hits your pharmacy shelf? It's not as simple as it seems. The journey from a researcher's hypothesis to human testing is riddled with surprises at every turn, but it's a story that remains under the radar for most of us.
Understanding this process is more crucial now than ever. With the race to develop vaccines and treatments for emerging diseases, the stakes have never been higher. Knowing how drugs are tested could change how we see our healthcare system. Get ready, because the truth is more intriguing than fiction.

You might assume that clinical trials are carefully organized, neat processes, but the reality can be chaotic, with unexpected obstacles at each phase. For instance, did you know that less than 14% of drugs entering Phase I trials ever make it to market? It's a gauntlet that even the most promising drugs often cannot pass. But that’s not even the wildest part…
Many believe that clinical trials are a luxury for first-world countries; however, a staggering number of these trials are conducted in regions with fewer regulations. This has prompted ethical debates about consent and the exploitation of participants. But there’s an untold aspect that differs drastically from what you might expect…
So, what happens next shocked even the experts. Strategies hidden in plain sight could disrupt not just the pharmaceutical industry, but also how you view experimental treatment itself. Keep reading, as the next chapter shifts everything you thought you knew about clinical trials.
Preclinical trials are the unsung heroes of the drug development process. Before any human testing occurs, researchers conduct laboratory and animal experiments to gather early efficacy, toxicity, and pharmacokinetic data. What might surprise you is how often these preliminary results can be misleading. Often, what's effective and safe in animals doesn't always translate into positive outcomes for humans. This discrepancy is a known but underestimated risk that complicates the entire trial process.

Despite being crucial, preclinical trials receive surprisingly little attention. Their failures and successes form the backbone of what later becomes human testing. Yet, they remain out of the spotlight, shrouded in scientific jargon and endless data sheets. This enigma around them leads us into a hidden world of painstaking detail and rigorous checks, which often make or break potential treatments. But there's one more twist to this tale…
Insider tips reveal that a company's decision to move forward with human testing often hinges not just on science, but on market potential and competitive landscape. This brings a corporate undertone into the world of medicine development that could shift perspectives or raise eyebrows. What you read next might change how you see this forever.
Despite this complexity, preclinical trials act as a critical filter, a necessary gauntlet that can determine whether further testing is justified. However, this is just the tip of the iceberg when it comes to the intricacies of drug development. The complexities deepen as we transition into actual human testing.
Phase I trials mark the first time a drug is tested on humans. Usually involving healthy volunteers, these tests focus on safety rather than efficacy, attempting to determine pharmacokinetics and pharmacodynamics in a human body. Surprisingly, the attrition rate is high, with nearly 30% of these trials failing due to safety concerns or lack of efficacy shown in humans.

What sets Phase I apart is the level of uncertainty. Volunteers are essentially pioneers venturing into uncharted territory with drugs that could have unpredictable effects. While conducted under stringent ethical regulations, the risks involved are more significant than most assume. This reality makes every participant a crucial puzzle piece in a giant scientific question mark. You won’t believe the hurdles that emerge next…
Despite this, Phase I trials are exciting opportunities for medical advancement. Participants often earn monetary compensation, but the real draw is the chance to contribute to groundbreaking treatments that could save lives. Their stories and experiences are full of insights yet rarely shared publicly. What lies hidden in these narratives could change perceptions drastically.
Phase I is just a stepping stone. There are layers of complexity and contentious factors that unfold as clinical trials progress. When unexpected side effects occur, they bring to light ethical conundrums and regulatory challenges. The implications are vast and shocking as you’re about to discover.
Phase II trials are where things get serious. Here, the drug is tested on patients who actually have the condition it aims to treat, allowing for an initial glimpse into its efficacy and side effects. Amazingly, only about 33% of drugs make it past this phase. Why is this? The reasons might surprise you.
One key factor involves the diverse responses from different patient groups. What works for one demographic might have a completely different impact on another, unveiling complexities that require adaptive trial designs and multiple study sites. Unveiled here are mysteries and surprises that challenge scientists in ways you wouldn’t expect. But the revelations don’t stop here…
Another hurdle is the ever-present placebo effect, which is particularly pronounced in Phase II trials. Researchers must meticulously design these trials to account for it, as it can sometimes overshadow the drug’s actual efficacy. These insights into human psychology reveal hidden layers into how and why certain treatments appear to work—or not.
In Phase II, the stakes are higher, as the science becomes an intricate dance of data interpretation and ethical determinations. Unseen by the public eye, each decision and outcome is fraught with implications not just for development, but also for broader healthcare paradigms. Wait until you see what happens in the next chapter—it's eye-opening.
Phase III trials effectively set the stage for a drug's future. Here, large-scale testing on diverse populations tests a drug’s efficacy, monitors side effects, and compares it to commonly used treatments. The tension? Up to 50% of drugs that get to this point don't make it to market, a reality unknown to many outside the pharmaceutical field.

This stage is often influenced by marketing interests and financial stakes, with pharmaceutical companies investing millions and sometimes billions. With these investments comes pressure to perform, and it's not uncommon for this phase to be gripped with what insiders call 'white coat syndrome'—where trial outcomes may be unintentionally biased to favor the drug. But wait, there’s more to uncover!
Unexpectedly, regulatory bodies like the FDA play a dual role. They’re not just gatekeepers of public health, but also influences in steering the trial designs, which can dramatically shift outcomes. Their decisions sometimes spark controversy, affecting market releases and public trust. This dimension of clinical trials is as intriguing as it is crucial.
Phase III is fraught with high stakes and complex ethical considerations. The success or failure of trials at this juncture can redefine medical practices and shift public health approaches. But nothing quite prepares you for what lies ahead when the trials conclude and approval becomes the new battleground.
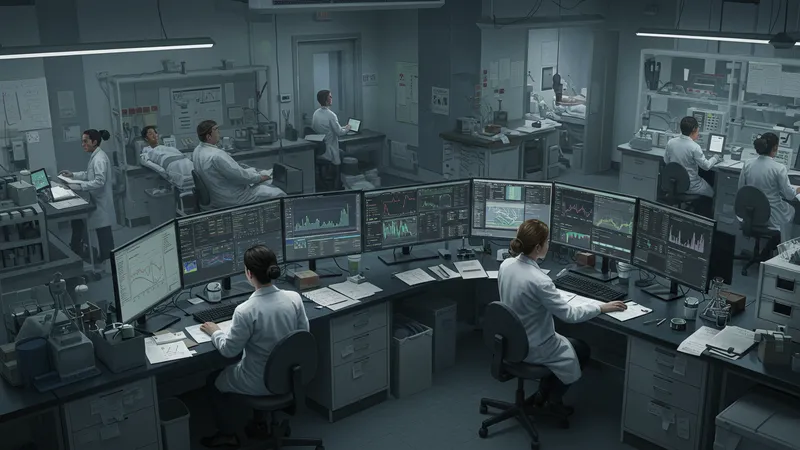
Once a drug completes its clinical trials, it faces regulatory approval—a formidable barrier not unlike navigating a labyrinth. Not all discoveries delight, as only about 20% of drugs that file for approval ultimately get the green light from regulators. What goes on behind closed doors could surprise even industry veterans.
The approval process involves thorough data scrutinization. Much of this data is examined in excruciating detail to ensure the drug’s benefits outweigh its risks. However, politics and industry lobbying inevitably find their way into regulatory environments, influencing outcomes in unforeseen ways. This labyrinthine network is cloaked in a veil of procedural rigor, yet it's far from impenetrable.
Often, drugs falter at the final hurdle not because they aren't effective, but due to concerns over safety or insignificant improvements over existing therapies. The fate of many potential treatments ends here, prompting heartbreaking decisions for both companies and patients in need. Just what does this all mean for future innovations?
For those drugs that do receive approval, the real-world impact begins to unfold. Clinical trials may end, but the journey for ensuring safety continues long after. So, how do these dynamics change how we understand the pharmaceutical landscape? There's another layer to this story that reshapes everything you thought you knew.
Even after a drug hits the market, the testing does not end. Post-market surveillance is key to identifying long-term effects that may not have appeared in earlier trials. Surprisingly, it's estimated that post-market studies reveal significant issues in about 10% of approved treatments, leading to label changes or even recalls.

This stage is a crucial aspect of ensuring public safety, but it often goes unnoticed by the general public. The act of ongoing surveillance is a testament to the importance of vigilant data collection long after clinical trials conclude. The discoveries made here can lead to challenges that pivot the narrative of a drug’s efficacy and safety drastically.
Pharmaceutical companies find themselves in a precarious position, balancing between transparency and business interests. The real-time monitoring of adverse effects can impact patient safety and the company’s reputation, making this a critical yet sensitive phase. But what unfolds in this stage often sparks innovative responses.
Patients and healthcare systems rely on these findings to make informed decisions. The constant monitoring uncovers realities for both drug manufacturers and users. Yet, in navigating this web, where do priorities lie, and what does that mean for the future of medical treatments? The implications are widespread and deeply impactful.
At every phase of a clinical trial, there is an underlying ethical framework meant to protect participants. However, ethical dilemmas are as common as they are complex. It's astonishing how sometimes ethical guidelines can be overshadowed by the urgency of medical breakthroughs and the allure of success stories.

One significant concern is informed consent, which sometimes becomes a mere formality instead of a comprehensive process. Ensuring that participants fully understand what they are signing up for is crucial, yet inconsistencies exist, leaving room for ethical ambiguities. How can this be, and what needs to change?
Another captivating dilemma involves the test subject selection, particularly in global trials where standards may differ across countries. Can the pursuit of quick results jeopardize ethical standards? This ongoing debate stirs emotions and calls into question the global implications of trial diversity.
Ethics in clinical trials are vital yet vulnerable to human error and corporate pressures. The consideration of what constitutes an ethical breach continues to evolve, forcing us to confront uncomfortable truths and re-evaluate practices. What next steps in ethical regulation may redefine the future of trials altogether?
Technology is transformative, even for the well-established protocol of clinical trials. Digital innovations are reshaping trials, from electronic data collection to AI-powered patient matching. Did you know that these changes can potentially reduce trial timelines by up to 30%? It's groundbreaking.

This transformation impacts every trial phase, streamlining processes and introducing efficiencies previously unimaginable. With real-time data capturing, professionals can make informed decisions faster, significantly influencing trial outcomes. Yet, how do these tech advances affect traditional methodologies?
Telemedicine and digital health records open new pathways for trials, particularly in remote and underserved populations. These avenues allow for increased participation diversity and real-world data collection, bridging gaps long ignored. But do these benefits come with added layers of complexity?
The rise of digital tools in clinical trials is just the beginning, hinting at a future where technology and medicine become inseparable. This shift stands to not just enhance but potentially revolutionize how we think about drug development and testing. Could the future of trials look dramatically different than we ever envisioned?
Funding is the backbone of clinical trials, often dictating their scope and speed. Amazingly, pharmaceutical companies spend over $2.5 billion for drugs to reach the market. But where does all this money come from, and who stands to gain—or lose?
Much of the funding comes from private entities, pharmaceutical companies, and occasionally, government resources. The struggle for resources can lead to competition and sometimes controversial practices, painting a picture of the industry rarely seen by outsiders. But what consequences do these financial pressures bring?
Costly endeavors often depend on securing patents for profitable returns. They can stifle smaller companies' ability to innovate, leading to industry dominance by a few key players. The role of these financial dynamics incites passionate discussions about fairness and accessibility.
The financial underpinnings of clinical trials remain a contentious aspect of the industry. The financial strategies uncovered could reshape how investors, companies, and researchers approach the dawn of new studies, affecting everything from trial scope to market breakthroughs. How does this landscape change the broader conversation about healthcare access?
Decentralized clinical trials are a rising trend aiming to increase convenience and accessibility for participants. Conducting these trials outside traditional research sites is an innovative approach offering significant flexibility. But their rise prompts an essential question: Are they as effective?

Proponents highlight the benefits of decentralized trials, such as reduced participant burden and wider geographic reach. This method has the potential to increase enrollment in studies, fostering a more diverse participant base. But alongside these perks, there are challenges to resolve.
However, decentralized trials also bring new complexities, such as data integrity and regulatory compliance concerns. While they can streamline patient involvement, they also raise issues about standardizing and securing data across various platforms and locations. But how can these challenges be met head-on?
Decentralization presents a frontier filled with promise and pitfalls. As they gain prominence, these trials stand to reshape the traditional framework, yet they must be approached with caution and foresight. Could this trend revolutionize trials, or are there hidden pitfalls that yet remain uncharted?
International trials expose cultural, ethical, and logistical differences that offer vibrant perspectives on drug development. Conducting trials worldwide introduces a spectrum of diversity that is crucial for comprehensive data analysis, but comes with its own set of challenges.

Cultural nuances affect participant recruitment and compliance, making it vital for teams to adapt approaches to fit local customs and laws. This cultural symbiosis enriches the data but also demands sensitivity and respect for varied backgrounds and legal frameworks. How does the global reach impact trial results?
The logistics of international trials are daunting, involving coordination across time zones and communication between disparate medical systems. Regulations often vary widely, requiring a nuanced navigation of political and legal landscapes. This complexity can obscure trial conditions, affecting outcomes and ethical considerations alike.
Despite these challenges, international trials hold promise for creating truly representative sample groups, potentially enhancing the robustness and applicability of findings. Embracing global diversity in trials is vital for future progress, yet the path is fraught with difficulties that may alter trial practices globally. What changes should be anticipated moving forward?
Pharmacovigilance is a critical aspect of post-market monitoring focused on drug safety and efficacy. Surprisingly, it can take years before adverse effects become fully understood, and when they do, the implications ripple across the pharmaceutical landscape.

This vigilance stems from reports by healthcare professionals and patients, feeding into rigorous databases for analysis. However, reporting systems can be inconsistent, often leading to delayed revelations of side effects. Traceability and transparency are key but remain constant challenges. But what strategies are employed to address these gaps?
The marshalling of safety data is paramount to public trust and the sustainability of pharmaceutical innovation. Robust pharmacovigilance efforts have led to notable recalls and safety updates that protect the public, yet they also instill caution in ongoing and future trials. What does this mean for long-term regulatory practices?
As the focus on safety in medical treatments deepens, the expanding domain of pharmacovigilance offers reassurance. Yet, the persistent search for safer, more effective medications propels this field forward with urgency, redefining how risks are managed in an evolving healthcare landscape. The dialogue around risk, efficacy, and vigilant oversight continues to evolve as you ponder its future potential.
After traversing the complex journey from hypothesis to human testing, it's clear that clinical trials are a dynamic and multifaceted process filled with challenges and breakthroughs. Each phase unveils new intricacies and ethical considerations that shape the landscape of drug development.

Whether it's understanding the meticulous nature of preclinical studies or grappling with the ethical dilemmas in human trials, every step presents a unique opportunity to redefine modern medicine. What might start as a single hypothesis ultimately impacts lives on a global scale.
Today's advancements in technology and global collaboration are paving the way for more efficient and inclusive trials. The dialogue continues to grow about how these practices can evolve to better serve humanity with safe and effective treatments.
This odyssey through clinical trials isn't just about science; it's about humanity's future and our commitment to health innovation. Don't keep this insight to yourself—share this story and broaden the understanding of what it truly takes to bring a life-saving drug from idea to reality.